News
» Go to news mainDalhousie Biomedical Engineering Students and Researchers Deliver Groundbreaking Solutions

Curing an Incurable Cancer
In Canada, 27 people are diagnosed with brain tumours each day, and an estimated 50,000 Canadians are currently living with the devastating condition. These cancers affect both children and adults, and often have low survival rates. Aggressive treatment options are available such as surgery, radiation and chemotherapy, however, current standards of care have failed to advance in decades.
This is partly because the brain is a critical organ and poses unique barriers for physicians and surgeons. This includes difficulty accessing the tumours during surgery and difficulty efficiently removing the tumour mass without compromising healthy tissues. 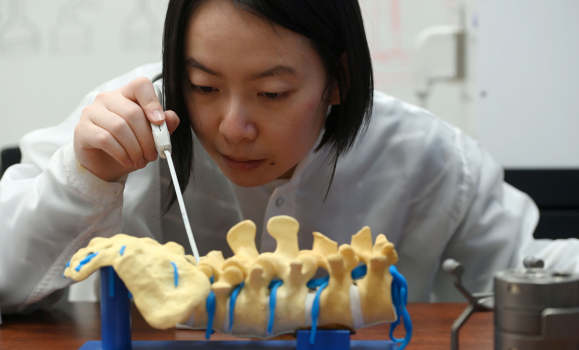
Over the past decade however, researchers and students from Dalhousie’s School of Biomedical Engineering have been pushing the boundaries in brain cancer treatment. Led by Dr. Jeremy Brown, the team has designed the world’s first high-resolution endoscopic surgical and imaging probe. It uses an ultrafast imaging platform to allow surgeons to see brain tumours with ten times the resolution of conventional imaging such as MRI and CT scans. The 3mm-by-3mm device is inserted through a small keyhole created in the skull and allows surgeons to follow an exact path to the tumour so that it can be surgically removed.
While the probe itself is already a first of its kind, Brown is now working on a secondary feature for the device; a therapeutic tool that will non-invasively vaporize cancerous tissues with high-intensity sound waves.
“You’ll be able to image and treat tumours at the same time. This is ground-breaking research,” he says. “These brain tumours are universally fatal, so the question now is, can we cure an incurable cancer?”
Brown, who is an associate professor in the School of Biomedical Engineering and the Department of Electrical and Computer Engineering, was inspired to create the device after his PhD supervisor was diagnosed with a brain tumour over ten years ago.
“My PhD. Supervisor, Dr. Geoff Lockwood, was diagnosed with a glioblastoma brain tumour and given just 1-2 years to live following surgery,” says Brown. “When he told me that his cancer was terminal, I couldn’t believe that there was nothing that could be done. As a result, I started to look into this particular pathology more and more to see what improvements in treatment and patient survival could be made.”

Today, Brown and his group of graduate and undergraduate students have begun conducting tests with the therapeutic probe. The device uses sound to induce bubbles in tumors that mechanically rip cancer cells into small fragments. It also offers a much greater level of precision and effectiveness than other forms of treatment such as radiation therapy.
Brown is also collaborating with immunotherapy professors at Dal to look at how the body’s immune system could respond to this new form of ultrasound ablation.
“When tumours are disrupted, they release antigens that trigger an immune response, so the next step it to ablate some of these tumours and then combine it with immunotherapy,” he says. “There is have been several preclinical studies and one clinical study for liver cancer by groups outside of Dal that have demonstrated the positive immune response from this new therapeutic technology. After ablating primary liver tumours, all of the other secondary liver tumours shrank because of the stimulated the immune system.”
Over the past year, students enrolled in the School’s Certificate of Biomedical Engineering program have been working on a variety of applications to improve the efficacy of the device. This includes developing new micro-fabrication processes to build ultrasonic imaging and therapy devices.
“Undergraduate student groups have worked on developing new electronic hardware for the imaging and therapy system and the odd group would work on developing software for the imaging probes,” says Brown. “I have had really stellar students from Electrical and Computer Engineering and most of my graduate students are recruited from this program.”
Brown says students working on the research project benefit from the school’s unique, multidisciplinary training environment, which he adds is viewed as an enormous asset by industrial and academic recruiters.
“All these skills are highly sought-after in growing sectors of the economy such as the semiconductor and med-tech industries,” he says. “Most previous graduates from my lab have gone on to work in fast-growing start-ups developing new biomedical devices.”
From One Innovative Device to the Next
Nearby, students in Dr. Robert Adamson’s lab are also contributing to cutting-edge research using an emerging imaging technology called optical coherence tomography (OCT).
Adamson’s group has pioneered the use of OCT to obtain high resolution images of the middle ear. While middle ear problems are common, they are often difficult to diagnose because current imaging tools don’t allow physicians to see past the eardrum. Often conditions such as conductive hearing loss are not properly diagnosed until patients are in the operating room, and surgeons have cut and lifted the eardrum out of the way.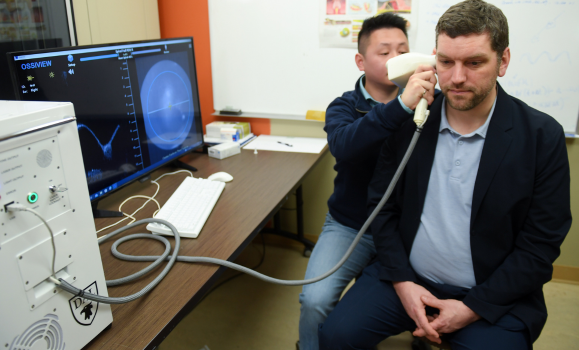
Adamson, a Professor in the School of Biomedical Engineering and the Department of Electrical and Computer Engineering, has been developing OCT for the middle ear over the past decade. He says the technology can see through the eardrum to produce high resolution images of the ear using safe, non-ionizing light. The device also provides physicians with the ability to measure the vibrations of middle ear structures caused by sound. This lets doctors identify problems that block sound from getting into the inner ear and cause hearing loss.
“In comparison to cancer, heart disease and other problems that can lead to death, hearing loss is often overlooked by biomedical engineers, but it can have a huge impact on quality of life,” says Adamson. “We want to make sure that ear surgeons have the diagnostic imaging tools they need to make good decisions about treatments that can improve patients’ lives.”
“Right now, doctors can look at the eardrum with a microscope, but they can’t see through it into the middle ear. Imaging technologies like CT and MRI are used, but their low resolution makes it difficult to see the tiny structures in the middle ear and CT exposes patients to substantial radiation. We want to provide doctors with a tool that they can use in their clinic, safely that gives them a preview of what they’ll find in surgery.”
Adamson and his team are now exploring how OCT can be used to diagnose a variety of different middle ear diseases to help ear surgeons better plan surgeries and counsel patients.
“We believe that OCT can play a role in the diagnosis of many middle ear problems including ear infections, otosclerosis, hearing loss from head injury and cholesteatoma. There may even be a role for OCT in planning and guiding robotic surgeries which are becoming increasingly common in the ear,” says Adamson. “We launched a startup company, Audioptics Medical that is working on commercialization the technologies we developed in my lab. The company is on track to have the system on the market by next year.”
Today, Adamson has three graduate students working on his research project and has had dozens of undergraduates work on Capstone projects related to hi work. He says his undergraduate students have played an important role contributing to areas such as software, mechanical design, benchtop testing and patient testing.
“In addition to engineering students, we’ve had medical students, surgical fellows and audiology students make contributions in developing and testing the system. I’ve found that engineering students love the chance to work with students in other disciplines on a project with clear patient impact,” he adds.
This year, 45 engineering students are set to graduate from Dalhousie’s Certificate in Biomedical Engineering program. Adamson, who along with his research work, is also the Coordinator for the School’s Certificate program, says the program is gaining popularity as students began to learn more about the versatility of the field.
“When I first arrived in Halifax fifteen years ago there were only a handful of biomedical device companies. Now, there is a whole ecosystem for the biomedical industry and several major success stories, many of them started by Dalhousie students,” he says. “At the same time, interest in biomedical research and the number of opportunities available for undergraduates with an interest in biomedical engineering has never been higher.”
He adds that as the healthcare systems continues to evolve, biomedical engineers will find more opportunities to apply technology to patient care. “This is why I think there are so many startup companies being created – there are a million places where engineering principles could be applied to healthcare to let doctors do their jobs better and to improve the lives of patients.”
And because of the rapid growth of the biomedical sector, Adamson says there are now plenty of great opportunities to start a career in biomedical engineering right here in Halifax.
“The feedback I’ve gotten from student in the certificate is that they really enjoyed working on biomedical Capstone projects. The process of interviewing doctors to understand their needs and those of their patients and to translate them into an engineering solution is very satisfying. It’s also feels great to work on a project that can potentially make a real difference in people’s lives.”
Recent News
- Blending the magic of engineering at the happiest place on earth
- Hands‑On Learning in Action: Students Gear Up for Peter Gregson Robotics Design Competition
- 2024 Engineering Golf Tournament
- Dalhousie Honours Dr. Ted Hubbard for Excellence in Educational Innovation
- Empowering youth and transforming communities: Celebrating International Women in Engineering Day
- Hydrogen Applications Research Lab Tour
- Unlocking the power of green hydrogen
- Deputy Prime Minister Freeland Champions Federal Research Investments at Dalhousie's Water Quality Lab
