News
» Go to news mainBiomedical Engineering Professor Helps Improve Lives of Cancer Patients
There are over 250,000 primary brain tumors diagnosed worldwide each year. While treatment options often include aggressive approaches such as surgery, radiation, and chemotherapy, Dr. Jeremy Brown is hoping to use new guided therapeutic methods for improving the lives of cancer patients.
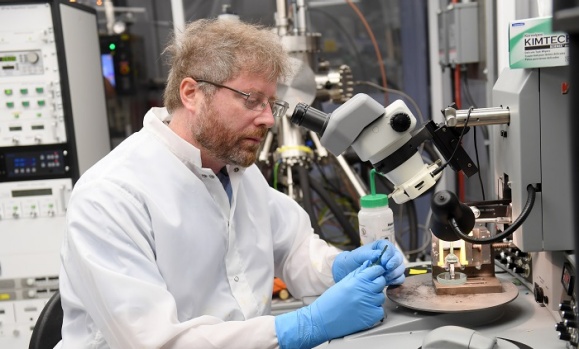
An associate professor in Dalhousie’s Department of Biomedical and Electrical Engineering, Brown has been working on new ultrasound technologies that will detect and fight off cancer cells using minimal invasive techniques.
Brown and his team have developed a cutting edge surgical and imaging probe aimed at improving cancer diagnostics within the brain. The tiny endoscope, which is the world’s first high-resolution endoscopic surgical and imaging probe, will be used for cranial procedures and will allow doctors to insert the device into a small keyhole drilled into a patient’s skull and diagnose conditions such as tumors.
Brown, who has been developing next generation ultrasound imaging and therapeutic technologies at Dalhousie since 2008, says he hopes to have the device in operating rooms within the next year, but he adds that there’s more to come for the miniature endoscope.
He says what makes the device truly cutting edge is the development of what he calls an “ultrafast” ultrasound platform.
What does that mean?
The technology will allow for novel surgical guidance modes, such as functional brain imaging, during “awake” neurosurgeries. Using the endoscope, doctors will have the ability to see the brain light up in certain areas when activated.
“This is really exciting because these surgeries are normally performed when the patient is awake. So when planning your surgical route, you can ask the patient a series of questions while applying electrical probes to the surface you are about to cut. If they can’t remember something for example, doctors will know that they can’t cut that area of the brain and will move on to another spot,” explains Brown. “So using functional ultrasound, doctors can map out large volumes that were activated when asked questions, and plan a route for surgery.”
In addition, Brown says his lab is also hoping to combine a therapeutic component to their endoscope allowing for the vaporization of brain tumors.
“These next generation ultrasound cutting technologies can create cavitation bubbles in the tissue, and when they pop, the tissue is vaporized,” he says.
Although the surgical technique is in clinical trials for treating liver cancer from outside the body, Brown says his team has miniaturized the technology with the intent of combining it with the endoscope for intra-surgical use.
“This is something no one else has done.”
Although the endoscope and therapeutic device are working independently, the next step will be combining the two technologies together.
“But before that can happen, we have to make a couple more technological advancements,” says Brown. “It could take another couple of years to have a fully integrated device that does both imaging and therapy.”
“There’s nothing like these, at this size, anywhere in the world,” he adds. “So to have a high resolution imaging endoscope that’s 3 millimeters in size and then an ultrasound cavitation device that’s also about 4mm in size, is magnitudes smaller than anything else that’s out there.”
Recent News
- Transforming plastic waste into 3D printing material
- 2024 Capstone Poster Expo
- Brewing Sustainability: Dalhousie’s Capstone team utilize algae for carbon capture project
- Capstone team helps local company reduce carbon footprint
- Engineering Programs & AU Open‑House
- An international student’s perspective on Canada’s Iron Ring tradition
- Crafting a legacy: Ispeeta Ahmed’s Journey as a Schulich Scholar Leader
- Next Steps Series: Engineering International Student Panel
