Events, By Category and Date:
» Go to news mainConcussion ‑ Brain Awareness Week
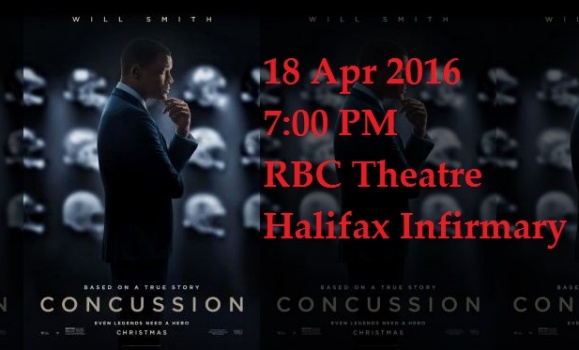
Free public screening with expert-led panel discussion afterwards.
Monday, April 18, 2016 (7:00PM)
QEII Royal Bank Theatre, Halifax Infirmary, Ground Floor, 1796 Summer St. entrance
Join the Facebook Page for this event
Moderator: Tim Krahn
Facilitators:
Frédéric Gilbert (Ethics, Policy & Public Engagement program, Australian Centre of Excellence for Electromaterials Science, University of Tasmania).Research topics:
• Neuroethics
• Mild traumatic brain injury in sport
• Ethics of novel invasive biomedical technologies, especially in the brain.
• Neuroimaging and neuropathologies
Kevin Gordon (Department of Pediatrics, Dalhousie University).Research topics:
• Pediatric neurology
• Concussion minor traumatic brain injury
• Clinical epidemiology
• Analysis of national databases
L Syd M Johnson (Department of Philosophy, Humanities & Kinesiology and Integrative Physiology, Michigan Technological University).Research topics:
• Neuroethics
• Concussion in athletics
• Disorders of consciousness
• Brain death
Recent News
- On what basis did Health Canada approve OxyContin in 1996? A retrospective analysis of regulatory data
- Matthew Herder Resigns from Patented Medicine Prices Review Board
- Permissive regulation: A critical review of the regulatory history of buprenorphine formulations in Canada
- Fair pricing of “old” orphan drugs: considerations for Canada’s orphan drug policy
- Podcast or Perish: Episode 040: Françoise Baylis
- Bioethicist Françoise Baylis asks why humans think 'they can just take everything'
- Killam Prize winners discuss research in Canada
- World‑renowned Dalhousie bioethicist and battery pioneer win prestigious Killam Prize

